Story Disclosure: This story is shared with the individual’s permission and reflects their lived experience. It is not medical advice and should not replace guidance from a qualified healthcare professional.
Sharing lived experiences within the BIPOC (Black, Indigenous, and People of Color) community is more than just storytelling; it is a vital act of resistance and a tool for bridging the diagnosis gap. When we share our journeys, we foster the solidarity necessary to ensure no one else has to navigate these uncharted waters in isolation. By bringing these narratives to light, we empower others to recognize symptoms, seek timely medical attention, and see their own reflections in a system that too often looks past them.
Nadine Kidd, a Black Jamaican American woman from Miramar, Florida, stands as a testament to this mission. Her life is a profound narrative of transformation, taking the fragments of medical trauma and systemic neglect and rebuilding them into a dedicated crusade for health equity.
The Early Battle: Diagnosis and Initial Symptoms
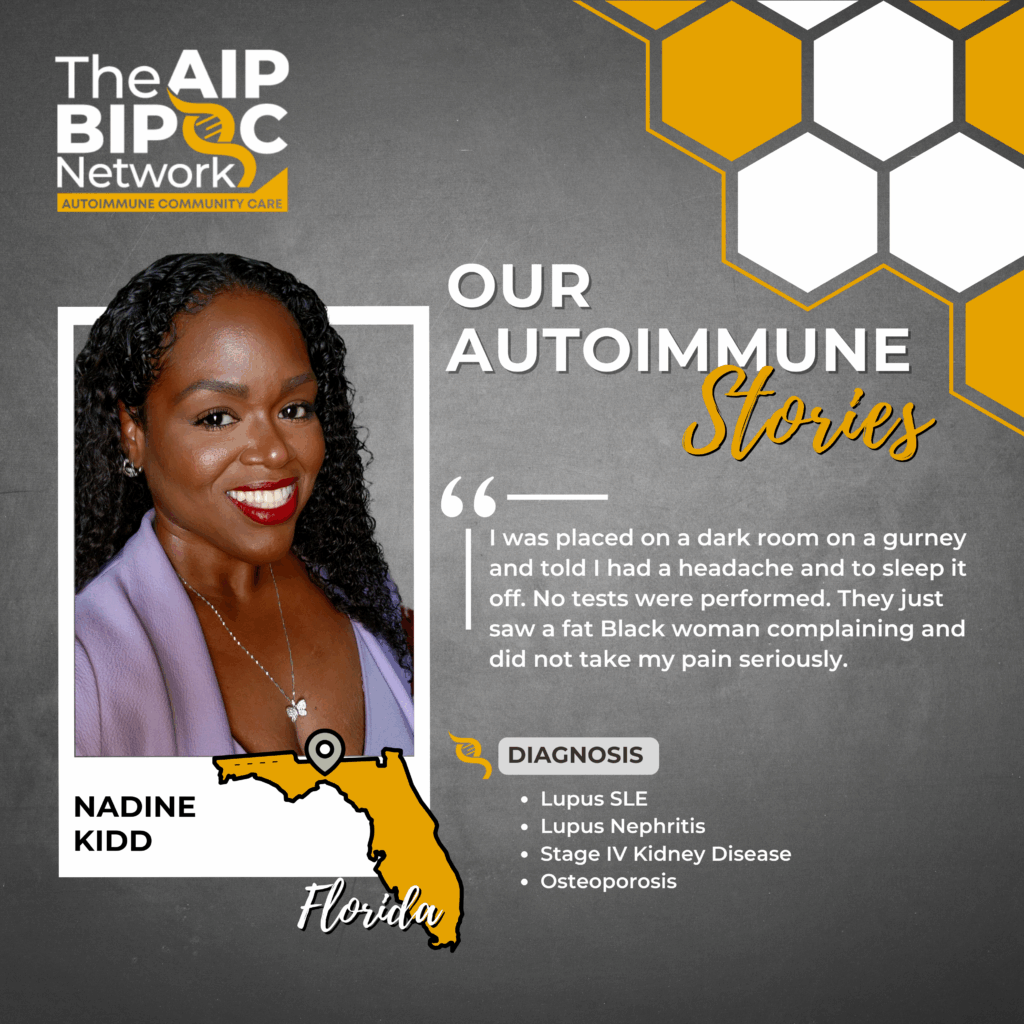
Nadine’s struggle began in childhood, though the names for her pain remained out of reach for years. By age 8 or 9, she was already enduring extreme arthritic pain, swelling in her hands and joints, and the telltale butterfly rash. Even then, the shadow of medical bias loomed large; because she was an overweight Black child, her pediatricians habitually dismissed her symptoms, attributing every complaint to her weight rather than investigating the clinical roots of her agony.
It was not until the age of 21, when the severity of her Lupus activity became impossible to ignore, that she received an official diagnosis. Today, Nadine manages a grueling profile of chronic conditions:
- Lupus SLE (Systemic Lupus Erythematosus)
- Lupus Nephritis
- Stage IV Kidney Disease
- Osteoporosis
The Shadow of Medical Neglect: A Crisis of Care
The most harrowing chapters of Nadine’s journey involve the repeated failure of “medical professionals” to provide basic human decency and care. Nadine reflects on the psychological toll of this systemic bias, noting:
“I was accustomed to mistreatment because of the color of my skin, and normalized it. I was used to being ignored.”
This normalization of neglect nearly cost Nadine her life during a brain hemorrhage incident. Rescued from work by EMTs and taken to an unfamiliar hospital, her screams of pain were met with indifference. ER doctors stereotyped her as a “fat Black woman” complaining of a mere headache. They performed no tests, placed her in a dark room on a gurney, and told her to “sleep it off.”
The failure of the safety net was absolute, and it was only the intervention of her sister that saved her. After the first hospital discharged her claiming she was “fine,” her sister drove her to a facility where her regular doctors had clearance. Within one brain scan, they discovered she was suffering from a brain hemorrhage and Meningitis, resulting in a two-month ICU stay. This pattern repeated when she suffered a stroke; EMTs misdiagnosed it as a TIA (Transient Ischemic Attack) and claimed she didn’t need a hospital.
Again, her sister intervened, ensuring Nadine reached the care that diagnosed her stroke and kept her hospitalized for a month. Throughout this decade of instability, Nadine also survived Sepsis and Pneumonia, complications that were exacerbated by a system that refused to see her.
The Physical and Emotional Toll of Treatment
The standard treatments for Lupus presented their own devastating trade-offs. To control her symptoms, Nadine was placed on high-dose steroids and immunosuppressants. These medications, coupled with kidney disease, caused her weight to balloon to over 480 lbs. She became morbidly obese, reliant on walkers and wheelchairs, and was eventually told she was on the path to needing a pacemaker.
The disease also stripped away her career in sales, a high-stress environment that triggered flares but provided her with financial freedom and a sense of purpose. Transitioning to permanent disability was a crushing blow that led to a deep struggle with depression and a reliance on multiple antidepressants.
“My biggest challenge was looking for a reason to not give up on life. My job gave me financial freedom… it made me feel productive and I had a purpose… But all that changed because of Lupus.”
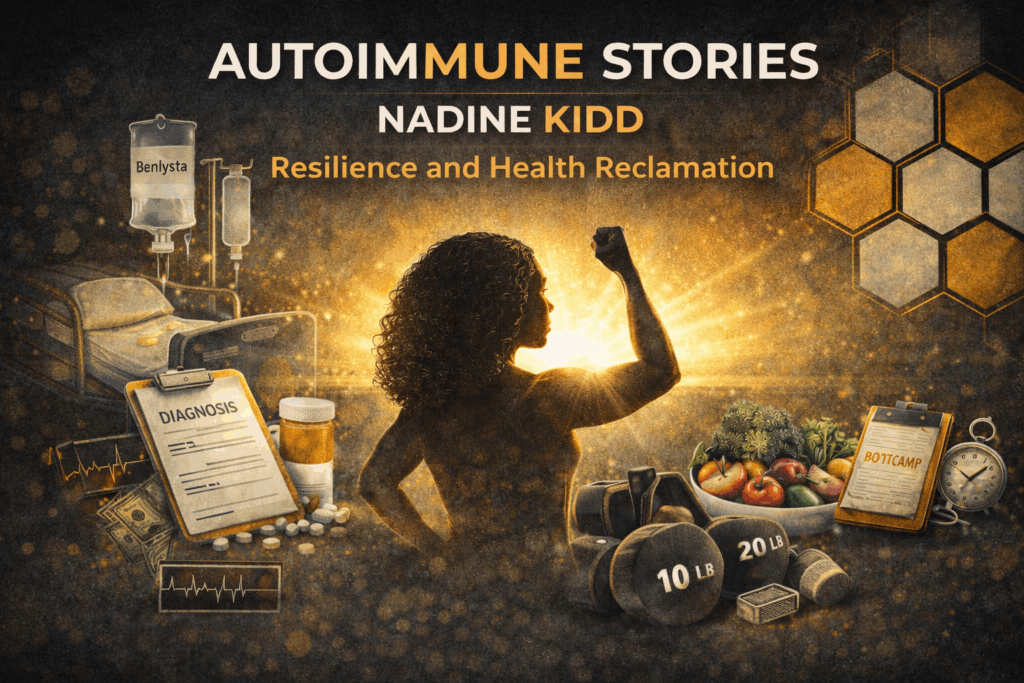
The Turning Point: Resilience and Health Reclamation
For the first ten years of her diagnosis, Nadine was trapped in a cycle of crisis, hospitalized three to four times every single year. The turning point finally arrived with the introduction of a new medication, Benlysta, which allowed her to finally taper off the high-dose steroids that had ravaged her body.
With a newfound glimmer of hope, Nadine reclaimed her agency. She overhauled her lifestyle, removing inflammatory foods and committing to a rigorous movement practice. She began attending a bootcamp with a personal trainer two to three times a week, focusing on mobility and strength. Her consistency yielded miraculous results: she has lost over 280 lbs and has maintained a seven-year streak without a single hospitalization.
Barriers to Access: The Reality of the Healthcare System
Even when life-saving treatments exist, systemic barriers often keep them out of reach for BIPOC patients. When Benlysta was released in 2011, Nadine was immediately denied coverage, a direct result of the “diagnosis gap” and the lack of People of Color in clinical trials. Because representation was so low, the FDA required a disclaimer stating the drug might not work for those of African American descent, which insurers used as a convenient excuse for denial.
Nadine navigated a gauntlet of systemic hurdles:
- Insurance Denials: Rejection based on the lack of POC representation in clinical research.
- Financial Exclusion: Even after approval, out-of-pocket costs reached $1,500 per month for the IV infusions.
- Step Therapy and Prior Authorization: Her rheumatologist spent months in a bureaucratic war, submitting biopsies and years of records to prove her need.
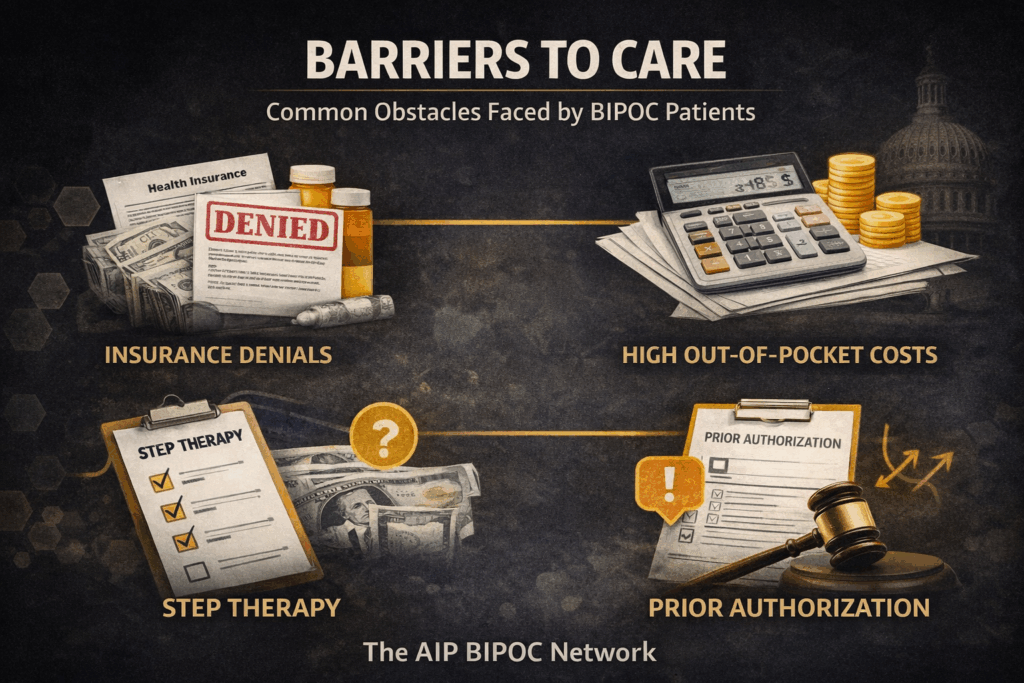
Nadine points to a perverse incentive within the system: she could only “afford” her medication if she was sick enough to be hospitalized for weeks, as those stays were the only way to hit her maximum out-of-pocket limits. This failure of the safety net meant that near-death experiences were her only currency for survival.
Channeling Anger into Advocacy
Nadine has transformed her anger into fuel, serving as an Ambassador for the Lupus Foundation of America (LFA) and GSK. She uses her voice to ensure that the “Safe Step Act” and “HELP Copays Act” become reality, meeting with State Senators and Congressional Representatives to put a human face on healthcare policy.
She is deeply involved in the LFA’s Clinical Trials group, working to fix the very representation gaps that led to her own medication denials. One of her most significant milestones was appearing in a national Benlysta commercial. Beyond the visibility, the experience was a profound emotional victory, helping her regain the confidence and sense of self that Lupus had once stolen.
A Call to Action and Advice for Warriors
Nadine’s journey reminds us that collective action matters. When we raise our voices together, we can push the healthcare system beyond passive “hearing” toward real accountability, and demand cultural competence that protects Black and Brown lives. To those currently in the thick of the fight, Nadine offers this advice:
“Don’t stop… find your why. Why to keep pushing, why to keep going, why it’s important to not give up.”
Jamie Nicole is the Founder and CEO of The AIP BIPOC Network. She is a Certified AIP Coach, patient advocate, and fitness instructor living with multiple autoimmune conditions. Jamie is committed to advancing equity, access, and representation for Black, Indigenous, and People of Color navigating autoimmune and chronic illness. Through education, advocacy, movement, and community-driven initiatives, she works to ensure BIPOC voices are centered in healthcare conversations and solutions.
Leave a Reply
© 2026 The AIP BIPOC Network, INc | EIN # 92-2526059 | all rights reserved | legal
